Blog
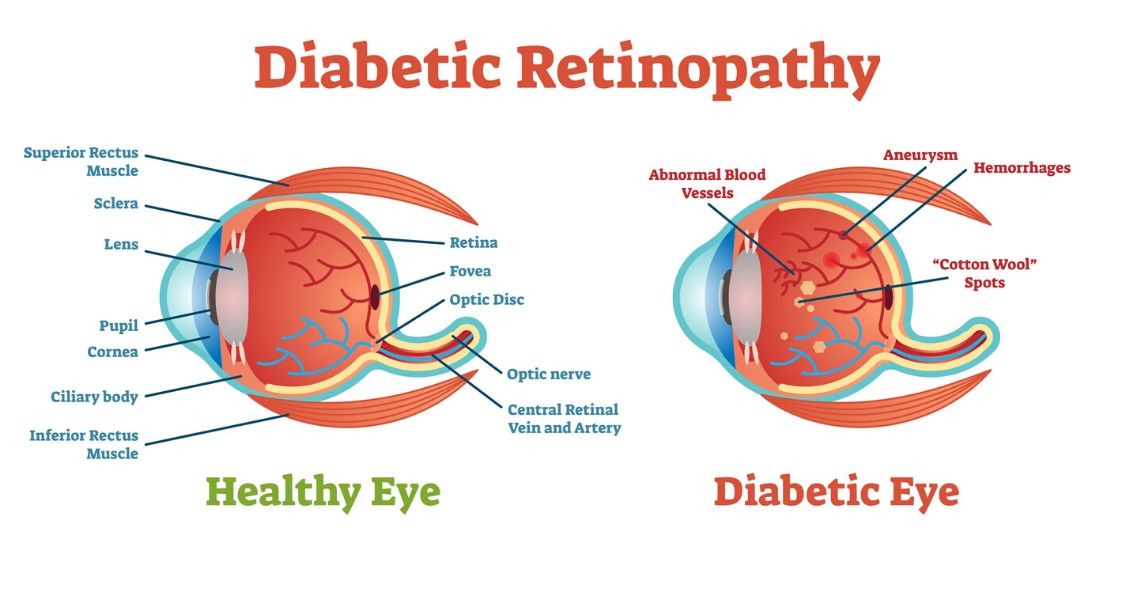
Diabetic retinopathy is an eye condition that can affect the retina of people who have diabetes.
The retina is the light-sensitive tissue that lines the back of the eye, and it detects light that is then processed as an image by the brain. Chronically high blood sugar or large fluctuations in blood sugar can damage the blood vessels in the retina. This can result in bleeding in the retina or leakage of fluid.
Diabetic retinopathy can be divided into non-proliferative or proliferative diabetic retinopathy.
Non-proliferative diabetic retinopathy: In the early stage of the disease, there is weakening of the blood vessels in the retina that causes out-pouching called microaneurysms. These microaneurysms can leak fluid into the retina. There can also be yellow deposits called hard exudates present in the retina from leaky vessels.
Diabetic macula edema is when the fluid leaks into the region of the retina called the macula. The macula is important for sharp, central vision...

There are certain eye conditions where an injection into your eye might be recommended.
Injections into the eye, specifically into the vitreous or gel-filled cavity of the eye, are called intravitreal injections.
In Part 1 of "You Want to Do WHAT to My Eye?" we talked mostly about anti-vascular endothelial growth factor (anti-VEGF) injections. Anti-VEGF injections are probably the most commonly injected agents and they are used to treat wet age-related macular degeneration (ARMD), diabetic retinopathy, and retinal vein occlusion.
But there are other injections that may be used as treatment.
Another injected medication used in combination with Anti-VEGF agents to treat wet macular degeneration, diabetic retinopathy and retinal vein occlusion are steroids. Additionally, steroids can be used to treat inflammation, or uveitis, in the eye. There is a steroid implant called Ozurdex, that looks like a white pellet and can last up to 3 months in the eye. The downside of...


